The Many Facets of Chronic Pain
By Dorthe Krogsgaard and Peter Lund Frandsen, Touchpoint, Denmark
Pain is a picture created in the brain. An abstract picture with many components. Alarm/stress is a main contributor to the pain picture, especially in chronic pain. In this article we will focus on decreasing the alarm. We present general treatment suggestions for chronic pain, and we focus on the heart as a great helper to break the alarm-anxiety-pain cycle.
But first, let us talk about reflexology techniques, should they be painful or not?
A Pain Pilot Project from the Touchpoint Clinic
During one week's treatments we hooked clients up to a computer program (emWave Pro from Heart Math Institute) showing the changing activity of the sympathetic and parasympathetic nervous system.
Via a small sensor placed on the client's earlobe, the computer registered the variation of the heart beats (Heart Rate Variability). The smoother the variation the more parasympathetic activity. 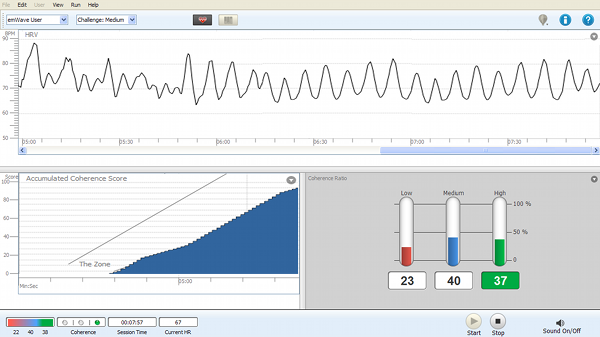
Conclusions of the Pilot Study
We were surprised by the significance of how clients deal with the impulses we provide.
The survey indicated that:
3 Important Take Away Points:
Chronic Pain is not Just an Extension of Acute Pain
Today, it is widely recognized among pain scientists that chronic pain is not just an extension of acute pain. Instead, it is viewed as a separate disease where the brain’s normal circuitry is rewired over a long period of time to deliver pain signals even when there’s no tissue damage or other obvious source of pain.
7 Key Insights on Chronic Pain:
Brain imaging studies reveal that chronic pain heavily engages the emotional brain. From a nervous system perspective chronic pain is very similar to an emotional experience.
Pain is always a personal experience shaped by previous encounters and influenced by biological, psychological, cultural, and social factors.
Chronic pain often (some say always) coincides with chronic inflammation. Signalling molecules released during inflammation can directly excite free nerve endings.
Inflammation also stops pain. Recently scientists at McGill University in Montreal discovered that a healthy inflammation process helps shut off the pain signals when the healing phase is completed.
The central nervous system becomes hypersensitive to pain signals, contributing to the transition from acute to chronic pain.
Read more on central sensitization here: https://mailchi.mp/touchpoint/tpnews0523-657970
40% of obese suffer from chronic pain, and the pain they report is more severe, often intractable, seeking more medical attention and consuming more painkillers. https://www.frontiersin.org/articles/10.3389/fnhum.2020.00181/full
Among diabetics chronic pain is common (20% - 60%) - much higher than rates in the general population. Most often back pain and neuropathic pain in feet or hands.
Cortisol enhances pain perception by changing the way the brain processes pain signals. Stress also amplifies pain enhancing negative emotions - anxiety, fear, and depression.
This is because the part of the brain that interprets sensations (somatosensory cortex) is deeply interconnected with areas that regulate emotions and the stress response (amygdala, hypothalamus, and anterior cingulate gyrus)
Treatment Suggestions with Chronic Pain
When so many factors are involved with chronic pain, how should we approach the sessions?
In the first session we suggest focusing mainly on symptomatic treatment to decrease the pain. Although the effect may only last for 1-2 days, it will importantly establish confidence and optimism.
In the following sessions, you can go deeper and focus on alarm in the body.
Clarify Important Aspects of the Process:
Patience. Chronic pain requires more treatments than acute pain conditions. One crucial aspect to comprehend is that pain is a picture generated within the brain. Pain itself does not necessarily cause harm to the body. Our thoughts are conductors of the signalling substances in the body. If possible, gently touch the aspect of spirituality.
Symptomatic Treatment
Focus Touch
Start with simply touching the reflex of the painful area and let the client focus. An acknowledgement of the painful area.Nerve Reflexology + Deep Touch
Actual selection of nerve points and reflexes depending on symptoms.Regardless of technique, work with “good pain” pressure for a longer time - or until the client feels a reaction or connection to the local area in the body.
Decreasing Alarm
Focus Touch Phrenic Plexus (solar plexus in old reflexology tradition) Diaphragm Spinal cord/ sympathetic nervous system. Vagus nerve Heart (watch the video included below) To support a coherent heartbeat via a relaxed heart = decreased fight and flight response. Brainstem Hypothalamus - Pituitary - Adrenals
U-2-Do (self-help)
To decrease the feeling of powerlessness it helps having a few tricks to do at home:
Decrease/control alarm with longer exhalations. Meditation - or Quiet Moments. Ear: Stimulate the vagus nerve by massaging the concha of the external ear (area just behind the opening).
Work the Heart Reflex
Many reflexologists are reluctant to work the heart area, and that is a great shame. We find it highly useful in stress management, and to help reduce alarm and chronic pain.
The heart is so much more than a mere blood pump. The heartbeat influences all other bodily rhythms and the heart talks intensively to the brain. When the heart is feeling good (coherent heart rate variability) signals from the heart goes via the vagus nerve to many different higher brain centres. The result is better cognition, less fear and anxiety and therefore also less pain!
Here is an excerpt from Touchpoint’s webinar “Round about: The Heart” showing how we place and work the heart reflex:
Ryesgade 27
DK-2200 Copenhagen N
Denmark
Tel: (+45) 2575 7047
Email >